
PromarkerD is designed to predict the risk of developing chronic kidney disease
Advertorial
Current kidney tests are reactive
Fifty percent of patients with type 2 diabetes will develop chronic kidney disease (CKD).1,2 Current standard of care tests (eGFR and ACR) are reactive; they can only detect CKD when it is present, once kidney damage has already occurred.3
Studies have noted these current kidney tests are not good indicators of early-stage CKD.4,5 Current guidelines (e.g. KDIGO and ADA) discount the risk of kidney disease onset for patients with type 2 diabetes in the ‘green zone’.
However, clinical studies show people in this ‘low risk’ green zone are not ‘safe’: One in 11 will progress to CKD.6
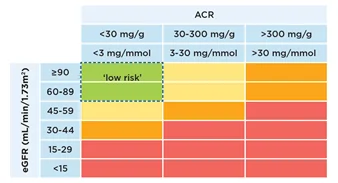
The PromarkerD test enables you to stratify the risk for your ‘green zone’ patients and provide better, proactive kidney health management.
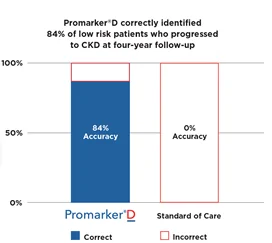
PromarkerD outperforms current standard of care tests. It accurately predicted renal decline at four-year follow up in 84% of ‘low risk’ (green zone) patients with type 2 diabetes. The current standard of care tests – eGFR and ACR did not identify any of these patients.6

Early CKD identification is essential for effective treatments to delay/prevent CKD progression and reduce cardiovascular risk.7
Promarker®D is proactive
PromarkerD is designed to predict the risk of developing CKD in the next four years in adults with type 2 diabetes with normal to moderately decreased kidney function.
The test system measures two protein biomarkers linked with kidney disease using enzyme-linked immunosorbent assay (ELISA). A clinically validated algorithm combines these results with clinical data (age and eGFR) to calculate the risk score in the proprietary PromarkerD Hub.
Test results and interpretation
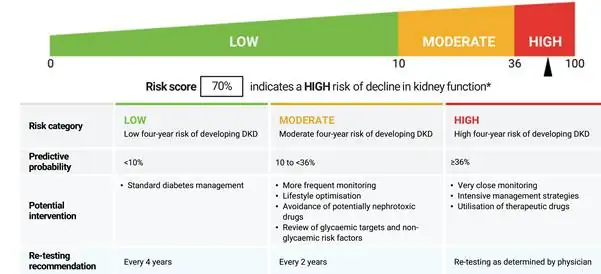
Manage your patients with confidence
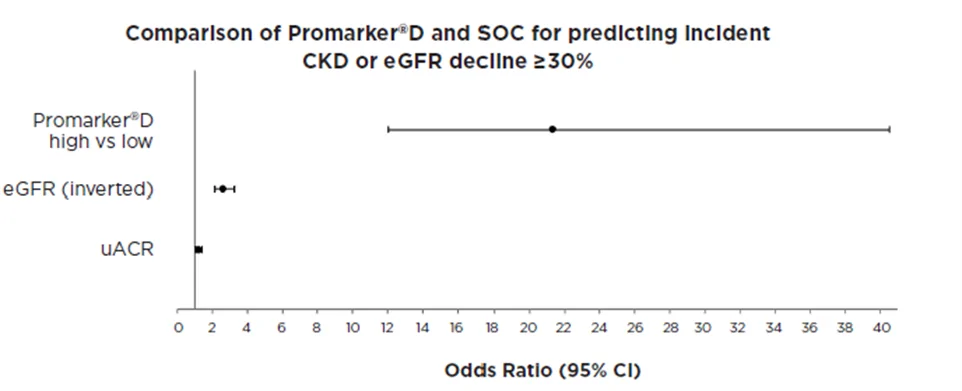
A study6 compared PromarkerD’s ability to predict kidney function decline with that of current standard of care tests (eGFR and ACR) in 857 adults with type 2 diabetes. The primary endpoint was incident CKD/eGFR decline ≥30%. At four-year follow-up, PromarkerD scores demonstrated a significantly higher predictive performance than standard of care tests (AUC 0.88 versus 0.63–0.82). Participants classified as high risk by PromarkerD were 21.34 times more likely to develop incident CKD than those it classified as low risk (p < 0.001). In contrast, participants classified as high risk under KDIGO risk categories (using eGFR and ACR results) were only 1.28 times more likely to develop incident CKD than those classed as low risk.
Learn more by watching this short clip below
Access the test today
Head to https://promarkerd.com/ to find out how you can access the test for your patients today or reach out directly to promarkerd@proteomics.com.au.
1 Thomas MC, et al. Diabetic kidney disease. Nat Rev Dis Primers. 2015;1:15018.
2 International Diabetes Federation 2021
3 Vaidya SR, Aeddula NR. Chronic Kidney Disease. [Updated 2024 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535404/
4 Lin, Chih-Hung et al. Early detection of diabetic kidney disease: Present limitations and future perspectives. World journal of diabetes vol. 7,14 (2016): 290-301. doi:10.4239/wjd.v7.i14.290
5 Swaminathan, Shilna Muttickal et al. Novel biomarkers for prognosticating diabetic kidney disease progression. International urology and nephrology vol. 55,4 (2023): 913-928. doi:10.1007/s11255-022-03354-7
6 Peters KE, Joubert IA, Bringans SD, Davis WA, Lipscombe RJ, Davis TME, PromarkerD Versus Standard of Care Biochemical Measures for Assessing Future Renal Function Decline in Type 2 Diabetes, Diagnostics 2025:15(6):662
7 Shlipak, MG et al. The case for early identification and intervention of chronic kidney disease: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney International, Volume 99, Issue 1, 34 – 47
